HPDP Case Study
HPPA 512 – HPDP
Case Study of Mr. Barry Anderson
Immunizations
Although Mr. Anderson stated that he received “a bunch of shots from a free clinic” last year, we are unsure which ones, or if he is reliable about actually seeking medical care. It would be safer to give him these immunizations:
-
- Td should be given since he mostly lives on the streets, and may use dirty needles with his heroin use.
- PPSV23 vaccine should be given because he is a smoker.
- Influenza vaccine should be given because it is November and the beginning of the flu season.
- Zoster, Meningococcal ACWY, and Meningococcal B vaccines should be given because he is MSM, which is an indication.
- He does not need Tdap, MMR, Varicella, Hep A, Hep B, HPV, and Hib because they are childhood vaccines. He does not need PCV13, because there should be a year between that and PPSV23.
Screening
-
- For this single visit, I would perform a Rapid HIV test. If he is positive for HIV, I would educate him about the dangers of it, that there is a confirmatory test that can be done, and if positive he should be given treatments to lower his viral load.
- I would also screen for alcohol misuse, tobacco use, and depression (see brief intervention).
- Anderson’s blood pressure is normal. I would inquire if there is any family history of cardiovascular disease. If not, I would not need to check further for HTN this visit. I also would not need to screen for obesity because he is underweight with a BMI for 15.8.
- For Mr. Anderson’s lifestyle, I would typically want to screen for Tuberculosis, Hepatitis B and C infection, Syphilis, Chlamydia, Gonorrhea, and Herpes, but I would mostly likely be unable to get the results within this single visit.
Health Promotion/Disease Prevention
-
- Injury Prevention
- Using condoms with all sexual acts
- Avoid using his used needles because they may be dirty or rusty
- Be aware of bed bugs (and street animals) to ensure a safe sleep environment
- Look both ways before he crosses the street
- If he gets behind the wheel, make sure to use a seat belt, and not be under the influence of alcohol or drugs
- If he owns firearms he should conceal them and not let them be easily assessable
- Diet
- I would make Mr. Anderson aware that he is underweight and let him know the risks that can come with it, such as malnutrition, decreased immune function, anemia, and osteoporosis. I would encourage him to try to eat more frequently, and make healthy choices that contain more nutrients and vitamins.
- Exercise
- Anderson did not disclose much about his physical activity, but I would assess his ability to perform exercises, and/or his physical restrictions. If he is mostly sedentary I would ask him to try to exercise a few minutes daily, gradually increase, and eventually work up to 150 minutes per week. I could suggest him to walk around more, job around, or utilize park gyms. I would also let him know that with increased physical activity, he may be able to work up a better appetite to eat, and gain weight.
- Harm Reduction
- Utilize the buddy system when using heroin
- Be strict with using the needles from needle exchange program one time
- Make him aware of heroin overdose protection programs in the area
- Make healthy choices when getting fast food
- Nicotine gum/lozenges
- Injury Prevention
Brief Intervention
Smoking Cessation
-
- “What do you smoke, and how much?” According to his reporting he smokes upwards of 5 cigarettes a day, which is ¼ of a pack. Assuming he has been “bumming them on the street” for 7 years (becoming homeless around age 23, and now currently 30), he has about 2 pack year smoking history.
- “Are you aware of what cigarettes can do to your health?” If he if unaware and willing to learn, I would let him know it can increase his risks of cancers, respiratory issues, bad breath, damaged teeth, and death. Also let him know it may be contributing to his weight loss and irritating the chronic cough he is experiencing.
- “Have you thought about quitting smoking?” “After you wake up in the morning, about how long after that do you take your first smoke?”
- “We can work together to help you quit. Would you be able to set a ‘quit date’? Have you considered nicotine alternatives like gums or lozenges?”
- “Quitting smoking can improve your health and save your money, because continuing the habit may get you hooked and start to buy packs for yourself” “Would you be interested in having a support group to go to?” “Can I schedule a follow-up date so we can talk about your progress made?”
Substance Use
It is especially important to ask these questions because I suspect that Mr. Anderson lost his job and apartment due to drug and alcohol use.
-
- “Do you drink alcohol? What do you drink? How many drinks would you say you have per week?” Mr. Anderson did not specify what he drinks and how much a week, but if I pressed him to tell me more, and he admits he drinks 5 or more drinks a day, I would try to counseling him more aggressively because he falls in the risky use group.
- I would ask him CAGE questions to get an idea if there is any alcohol abuse.
“Have you felt the need to cut back on your drinking”
“Have people commented or criticized your drinking, and you get annoyed at them?”
“Do you ever experience feeling guilty from your drinking?”
“Do you ever drink in the morning in order to stop shaking or recover from a hangover?”
If he responds to one of these questions positively, I would think he was at an increased risk. If he responded positively to two or more, I would think he is an alcohol problem and is at risk of abuse and addition.
-
- If he got a positive result on the CAGE questions, I would conduct the AUDIT questionnaire, skipping some that repeated the CAGE questions.
“How often do you have a drink containing alcohol?”
“How many drinks containing alcohol do you typically have when you drink?”
“How often do you have 6+ drinks per session?”
“How often during the past year did you find yourself unable to stop drinking?”
“How often during the past year did you forget or skip something because of drinking?”
“How often during the past year did you need to drink in the morning in order to stop shaking or recover from a hangover?”
“How often during the last year did you feel guilt from drinking?”
“How often during the last year did you forget what happened because of your drinking?”
“Have you or someone else been injured due to your drinking?”
“Has anyone expressed concern or suggested you to cut down on your drinking?”
Then I would calculate based on the AUDIT scoring system to see if I need to offer alcohol education, give advice, brief monitoring, and/or refer to a specialist or treatment.
-
- “Do you ever mix alcohol with your heroin use?”
- “Have you ever been drinking or using behind the wheel of a car?”
- “Besides heroin, do you do any other drugs?” I could also conduct the NIDA questionnaire.
“In the past year, how many times did you use alcohol, tobacco products, prescription drugs for recreational use, illegal drugs?”
If he says he has used any of these within the past year I would question further.
“In your lifetime, have you used cannabis, cocaine, prescription stimulants or opiods for recreational use, methamphetamine, inhalants, sedatives or sleeping pills, hallucinogens, street opioids, or other things”
If he says he has used any of these in his life, I would question further.
“In the past 3 months, how often did you use the substances mentioned before?”
“How often do you have the strong urge to use each drug?”
“How often does the usage of each drug lead to health, social, legal, or financial issues?”
“How often did you forget or skip something because of use of each drug?”
“Has anyone expressed concern or suggested you to cut down on your use of each drug?”
“Have you ever tried and failed to control, cut down or stop using each drug?”
According to the NIDA scoring system, I would assess the risk level of Mr. Anderson and conduct the respective recommendations.
“Have you ever used drugs by injection?”
Including an HIV test, I would recommend Hep B and C testing.
-
- “I would advise you to try to slowly lessen using these substances because they will have a negative impact on your health. Alcohol could lead to alcoholic hepatitis, liver cirrhosis, GERD, seizures, heart issues, and pancreas issues. Injecting drugs can lead to skin, joint, heart, and lung problems. They can be an opportunity to expose you to greater risk of infections. Also, alcohol and drugs may be another reason contributing to your weight loss.”
- “Have you thought about stopping drinking alcohol or using drugs?” “Have you tried cutting down on them in the past? What were some obstacles you came across?”
- I would counsel him against maladaptive thinking.
- “We can work together to help you quit. We can set a goal of how much you can cut down on your use of these substances if you would like? Would you be interested in having a support group to go to? Can I schedule a follow-up date so we can talk about your progress made?”
Depression screening
-
- This is important to do because people who drink alcohol and use drugs may be dealing with mental health issues. I would ask him if in the past two months did he, 1) experience little interest or pleasure in doing is usual activities, and 2) feel down, depressed, hopeless?
- If he agrees to the above questions, I may ask him further if he has suicidal ideations, anxiety, OCD, if he has ever seen a mental health professional. I would assess his situation and maybe let him know about the option of calling 311, or give him some referrals to mental health professionals.
Issues to Address:
-
- I would address his drug, cigarette, and alcohol uses first, and educate him of the harms that may come with it.
- Then I would counsel him on safe sex practices, educate on sexual diseases that may be risks for his lifestyle, and perform a Rapid HIV test.
- After, I would give the vaccinations.
- I would screen for depression, encourage him to exercise more, and give advice on harm reduction, along with how to have a better diet and prevent injuries.
- Finally, I would stress to him the importance of regularly being seen by a clinician, and ask if he would like to schedule an appointment to come back if a month to follow up.
Mini-CAT assignment
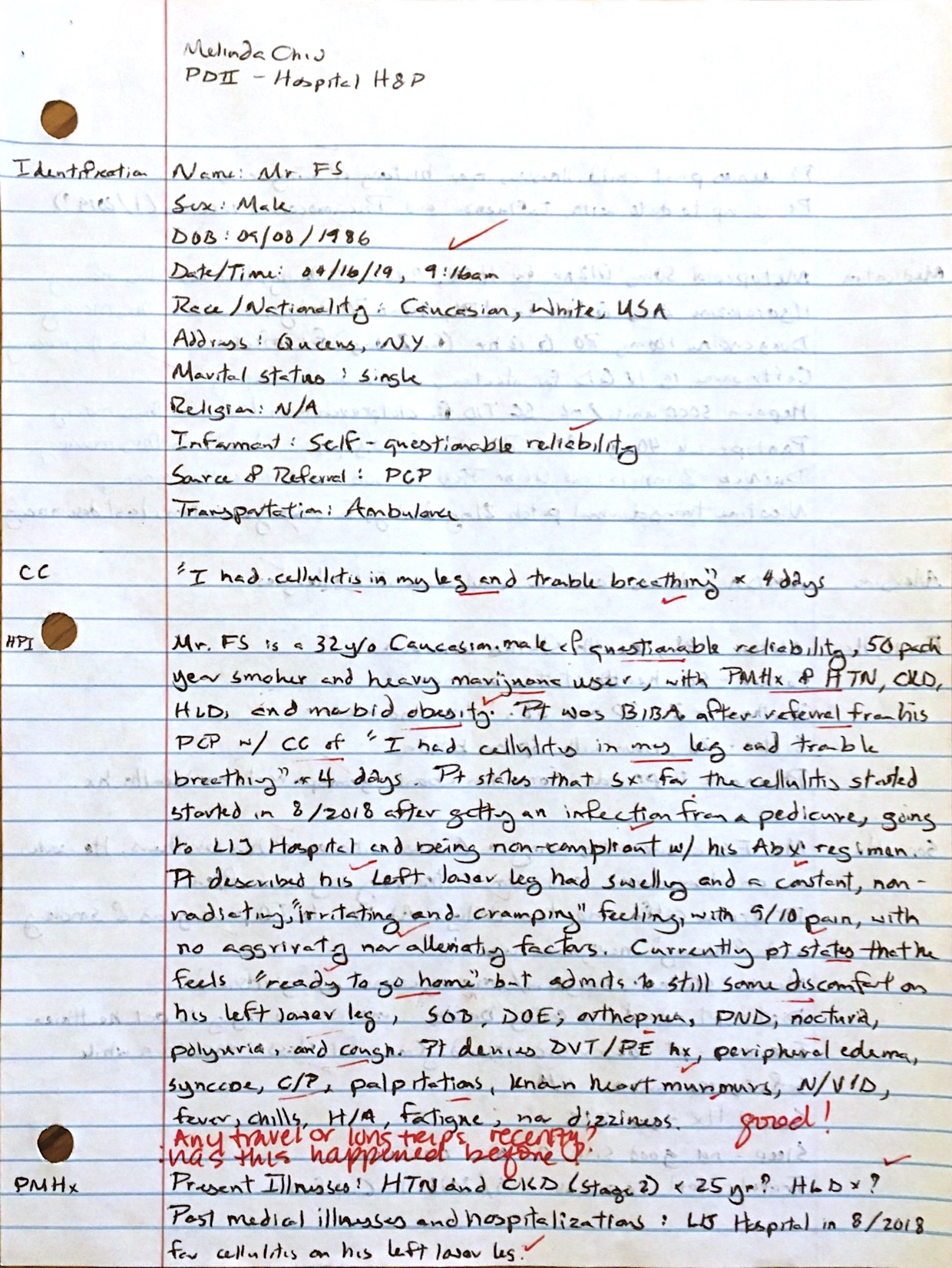
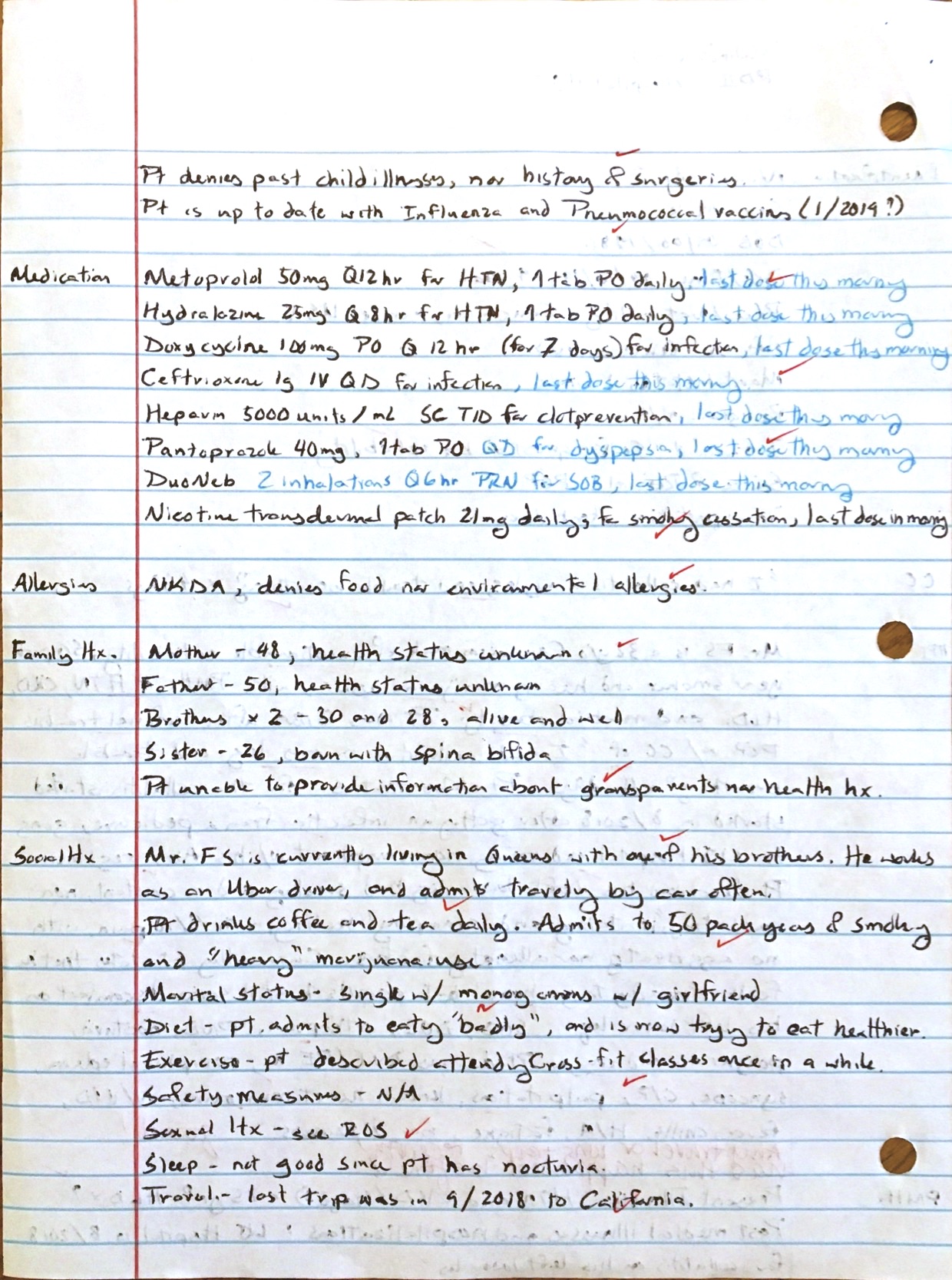
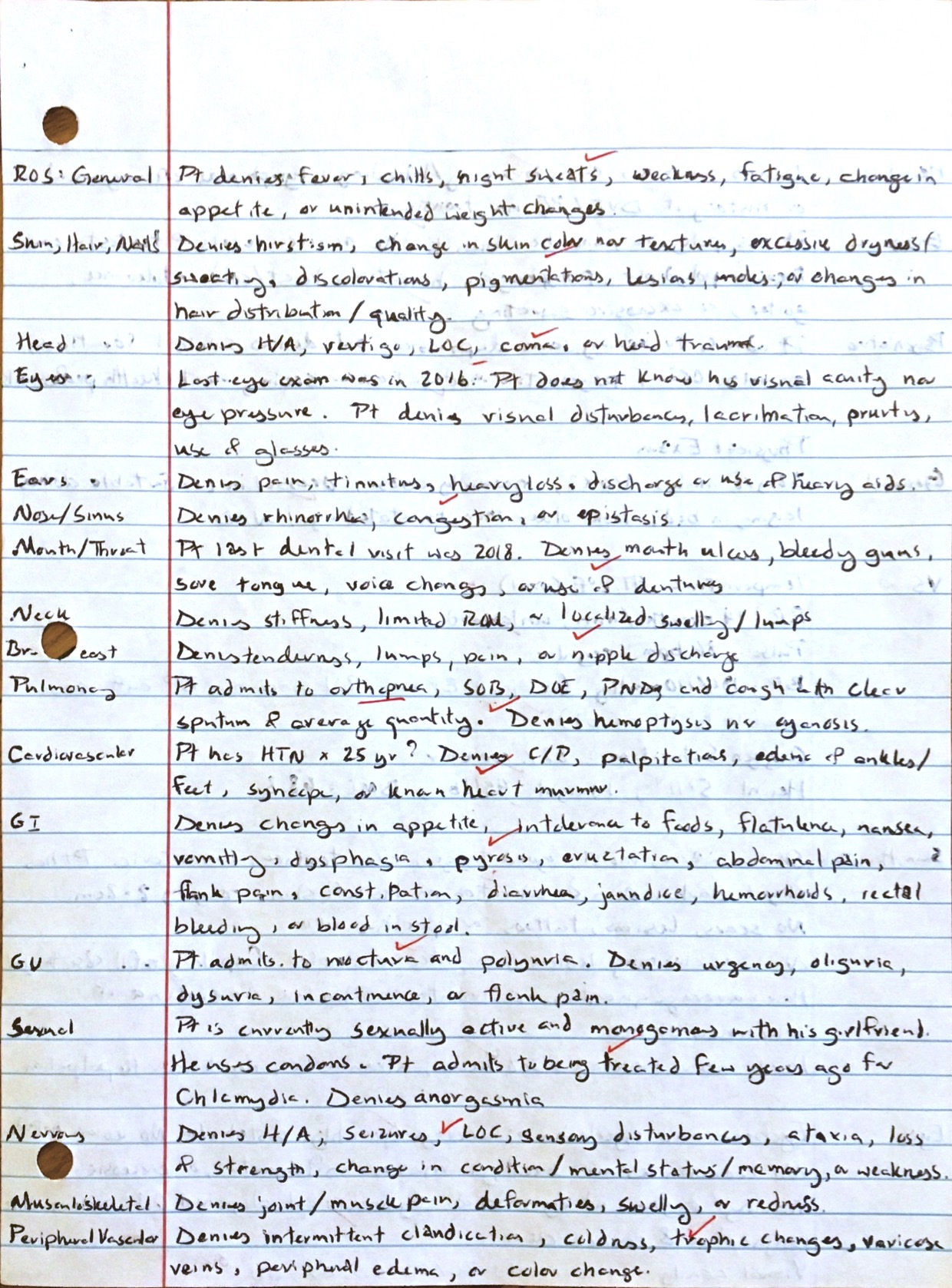
Fall 2018 vs. Spring 2019 H&P Reflection
- What differences do you note between the two H&Ps?
When comparing the earlier H&P to the more recent H&P, I noticed that within roughly the same amount of time given to work with the patients, I was able to cover more ground in the latter. I also can see how far I have come in terms of what I have learned in performing physical exams.
- In what ways has your history-taking improved? Are you eliciting all the important information?
My history-taking has improved by me being able to better draw information from the patient, and understanding what information is considered “pertinent.” This may be attributed to the interviewing skills and knowledge I have learned in class, and picked up along my hospital visits. Also, I gained more confidence and comfort with working with patients.
- In what ways has writing an HPI improved?
I believe that my HPI has improved in terms of thoroughness. I am better able to appreciate what parts of the HPI are more pertinent to cover and ask, according to different conditions and scenarios.
- What is your self-assessment of your current skill in performing a physical exam? Which areas do you feel strongest about/weakest about?
I believe that I have come a long way from where I started with knowledge on performing PEs. I am more comfortable with interacting and “touching” patients. I believe that I have a good grasp on what a routine PE entails, and understand situations where more in depth exams are warranted. The area that needs improvement, more experience, and comfort, would be performing exams on the more private regions of the body.
- Which of the specific areas will you target as needing particular focus in future patient visits when you start the clinical year?
In clinical year, I could use more practice in performing PEs in order to gain more knowledge and experience in medicine. I also look forward to learning more from the remainder of the didactic semesters in order to better form assessments and plans for my future patients.
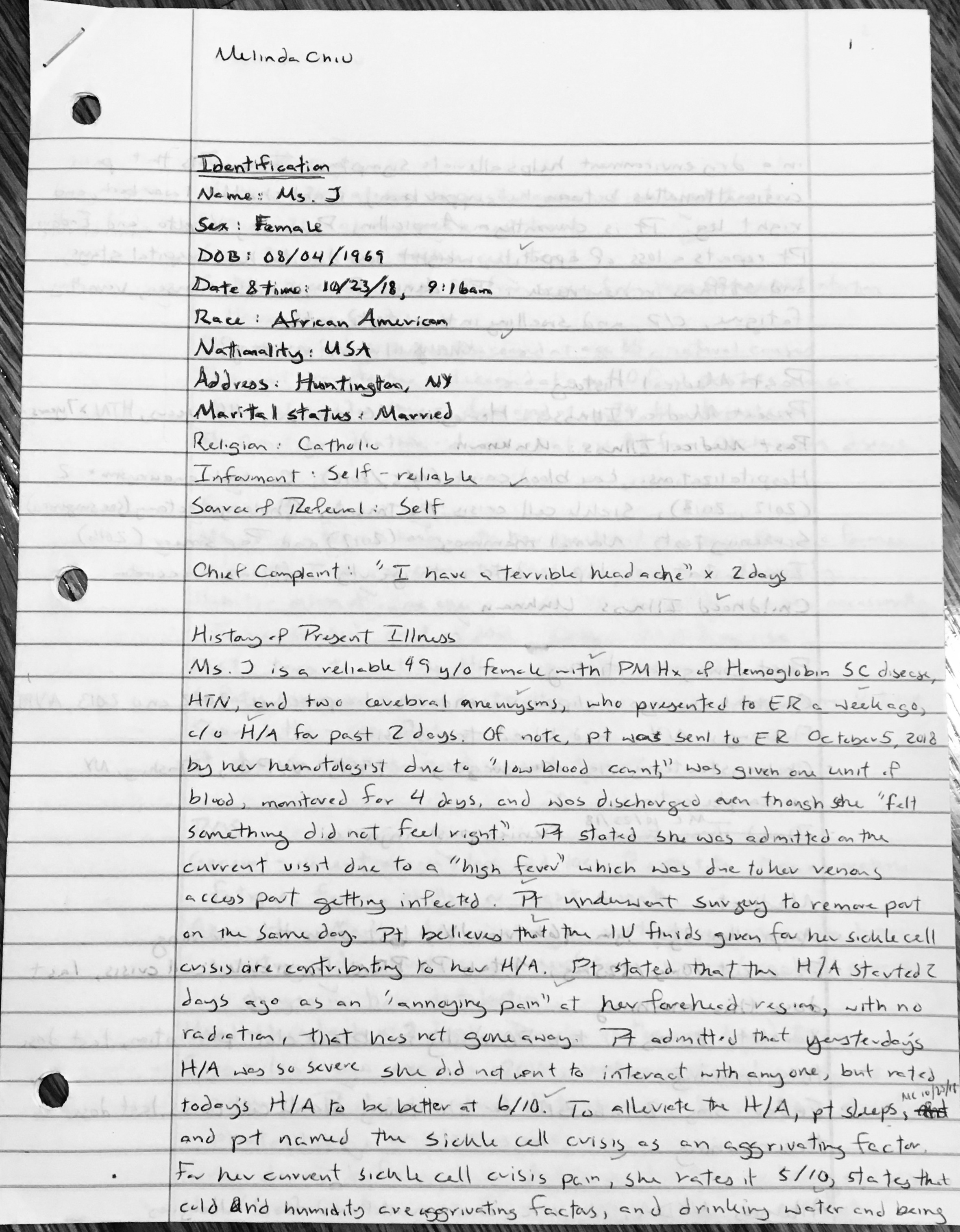
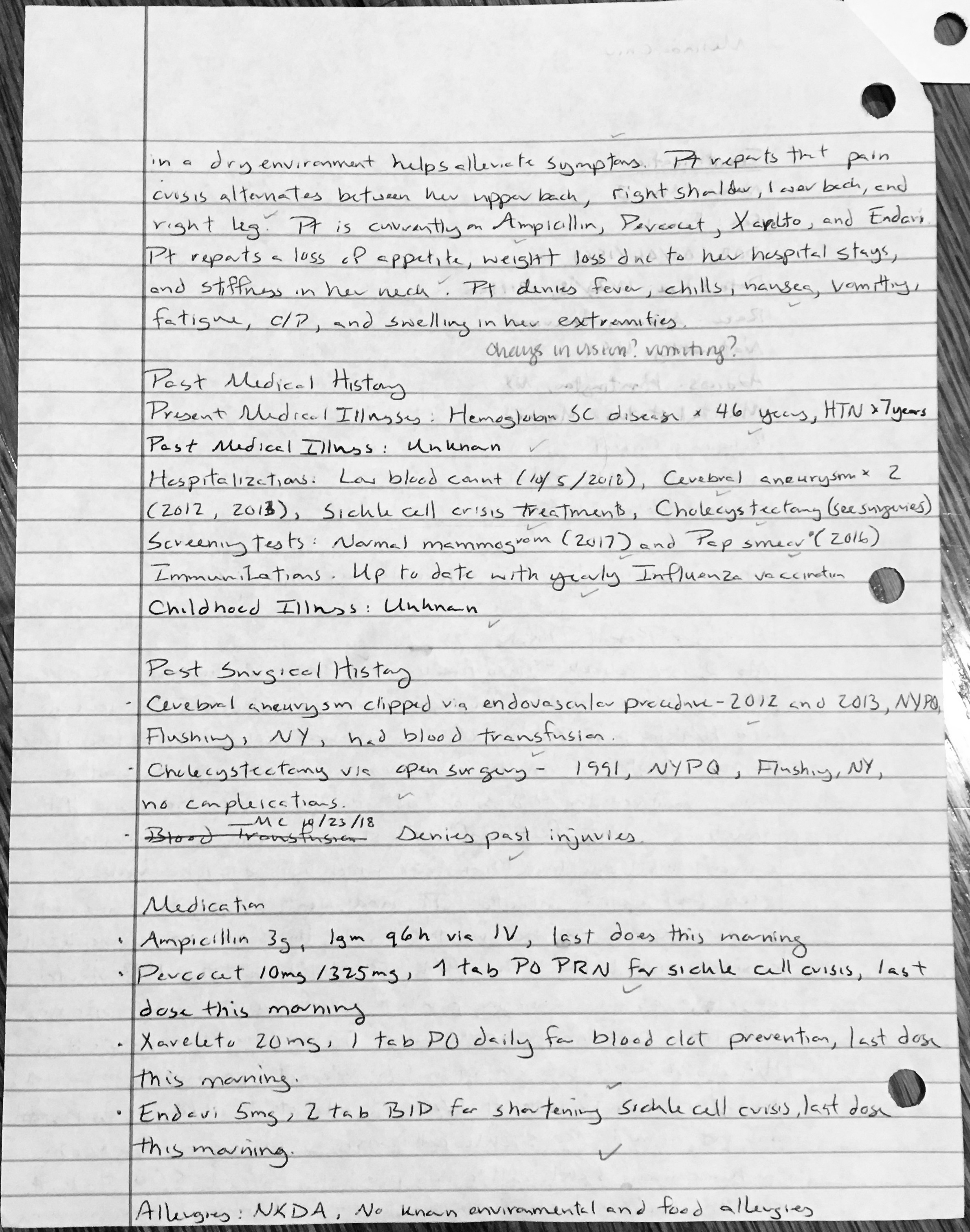
H&P From Spring 2019
Final Ethics Reflection on My Drive to Become a PA
12/11/2018
HPPA 514
Reflection Essay
In this piece, I will explain how I got my drive to become a PA, what I anticipate will be important aspects of my practice, and describe and explain how certain ethical principles play a part in the aspects I foresee.
In my junior year of high school, my father was diagnosed with liver cancer, and lost his battle with it a few months after. As I mourned my family’s loss, I had a chance to reflect on how my father’s medical team offered such a strong support network to my family throughout. I found myself looking up to every member, which aspired me to work towards becoming a PA. As I gathered more health experiences, my love for medicine grew. The PAs I met along the way were very knowledgeable, professional, enthusiastic about their profession, and formed strong relationships with their patients. My goal was repeatedly being affirmed, and I quickly realized my passion for becoming a PA was to make a difference; by giving back to the medical community, and to be able to treat and comfort patients and their families.
In my experience, knowing that clinicians and other healthcare staff truly cared for me and my family helped to decrease some stress and anxiety. I anticipate that in my practice, one of the most important aspects will be to understand my patients and their family’s healthcare expectations and beliefs. By spending time with them, I would be able to get to know them as individuals, and show that I care about them. By gaining their trust, it will only strengthen my ability to help and treat them. Another aspect that I find important is being able to volunteer. A PA I had come in contact with shared how she regularly volunteered to offer her medical services at sporting events. I was in awe of her selflessness, and the ability of PAs being able to help. Also, from knowing US is relatively advanced in medicine, I want to be able to travel to underserved countries to extend my services.
A key aspect for carrying out my vision is by forming strong relationships with my patients. I believe that the ethical principles of dignity, truthfulness, and beneficence will best support this in my practice. In the RCN report, treating patients with dignity was “to treat them as being of worth, in a way that is respectful of them as valued individuals”(1-pg8). This definition shows how it is essential to spend time to understand the patients on an individual level in order to build rapport, better treat them, and promote their dignity. Especially when I continue to serve patients in my practice or in volunteering, I will be faced with new cultures, values, and ways of living. Being aware and sensitive to this fact is essential. Ways to address this may be to respect patient’s space, explain and ask for permission for what I plan do in examinations, use caution when needing to expose body parts, and have compassion. Another important practice would be to learn about the patient’s preferences for disclosure; for example, if they want to be alone, with family or friends, nor not told much at all. This aspect ties in with the ethical principle of truthfulness.
In the Surbone article, truth-telling is described as “a dynamic, iterative, and interactive process that takes place between the [provider] and the patient, sharing many provisional truths in view of a common therapeutic goal(2-pg947). This explains how there should be a relationship where the patient’s goals, values, and cultural customs are appreciated by the provider. According to this mutual understanding, it will guide how “truthfulness” is shared. For example, cultures have different beliefs surrounding news of cancer. Some cultures believe that patients should know their diagnosis, while others may not disclose(2-pg946)(3-pg505-508). Beneficence can be seen on both sides of this scenario. It is defined as “caring about and for the well-being of patients, and working towards good of patient”(4-pg103). One culture may believe that the patient should be told the truth in order to make an informed decision for their next steps; while another culture may see that not disclosing the truth will protect the patient from unnecessary stress, and their clinician and/or loved ones should make decisions on their behalf(2-pg946). By spending time unpacking the patient’s expectations and preferences in health situations, I would be able tailor my methods to better care for and respect my patient’s wishes.
By practicing the ethical principles of dignity, truthfulness, and beneficence, I will be able to make a difference by better understanding my patients, and enhancing my services abroad.
References
-
- Royal College of Nursing. (2008). Defending Dignity
- Surbone, A. (2006). Telling the truth to patients with cancer: what is the truth?
- Tuckett, A. (2004). Truth-Telling in Clinical Practice and the Arguments For and Against
- Yeo et al. (2010). Concepts and Cases in Nursing Ethics – Beneficence
Patient Centered Interviewing
Balancing Autonomy and Beneficence in Healthcare
October 2, 2018
HPPA 514 – Biomedical Ethics
In healthcare, oftentimes ethics in considering treatments come into question. In this scenario, Mr. S asks for a prescription for Viagra despite an unremarkable physical exam and denial of sexual issues. Ultimately, the physician agreed to give the prescription. In this thesis I will use the principles of autonomy and beneficence to support my position in agreement with the provider.
Autonomy is defined as “the right [of the patient] to make independent decisions concerning one’s own life and well-being”(1) and “respect[ing] a patient’s moral personhood by honoring [their] carefully deliberated preferences”(2). Essentially, it is to let a patient consider what they want for their own treatment. Yeo et al.’s description of autonomy as “free action” supports this thesis. The patient voluntarily made the decision that he wanted Viagra, which is an aspect that ties into the patient giving informed consent, and respects patient autonomy(1). The patient did not express distress from pressures from his wife nor friend, nor did the provider offer this option. The only possible sources of persuasion could be from his perception of societal standards or expectations from the adult-film industry; however, these possibilities do not directly coerce the patient. Refusing to prescribe the medication would disregard the right of the patient to make his choice. He had his own desire to feel more masculine, hence, seeking for Viagra. Although he denied sexual dysfunction, there is a possibility of him feeling uncomfortable to disclose this issue. “Effective deliberation” in autonomy is another description that supports the thesis. This explains how the patient was able to express his desired goal of getting Viagra, with reasoning to “feel ‘more of a man”.” “Competence” is a concept that went hand-in-hand with effective deliberation, where a patient would need the mental capacity to make choices. According to the physician’s exam, it showed normal findings and had no remarks indicating that the patient was unable to make decisions for himself. Examining the concepts of free action, voluntary choice, effective deliberation, and competence under autonomy helps to support the thesis. The principle of beneficence also works in conjunction with autonomy.
Beneficence in healthcare is an ideology that describes “caring about and for the wellbeing of” patients, and the “orientation toward the good of patients”(3). In other words, it is a way of intentionally treating patients with actions that emphasize benefiting them and their outcomes. Even if some outcomes inevitably result in risk, beneficence will lean towards choices that produce more “good” than harm to the patient and/or others. In the case with our patient wanting Viagra, beneficence supports the physician. This is because the medication will not affect others negatively, and the physician predicted low-risk to the patient. One might argue that Viagra may harm the patient with side-effects, or mentally, if it does not meet his desired outcome, and therefore he should not be given the medication. This stance can be countered by the concept of “dignity of risk.” This idea explains that a person should have the dignity to be in command of assessing risks of what they desire, act on pursuing it, and be subject to consequences that may follow(2). In other words, although the patient’s choice may have risks, their choice should be respected. Another facet of considering treatment with beneficence places importance on the quality and sanctity of life(3). These ideas evaluate how a treatment is able to improve one’s life, and views that everyone’s needs and concerns should be given the same consideration and respect as everyone else’s. The patient wanted to improve his self image of masculinity, and believed that Viagra could help. The medication has the potential to improve his “quality of life” in this way. His concern is not far off from a patient wanting cosmetic surgery (e.g. breast augmentation), even though their condition is not life-threatening nor affects their physical health. This case shows how a procedure can be considered based on a patient’s desire for it, as well as for benefiting their mental-state and self-image. After all, the World Health Organization had defined health as “a state of complete physical, mental and social well-being,” which shows that the concept of “health” is multifaceted and all parts should be considered(4). The ideas of producing more “good” than harm, dignity of risk, quality of life, and sanctity of life, and the broad definition of health support the physician in prescribing the medication.
With the principles of beneficence and autonomy, I have supported my argument in having the provider write the prescription for Mr. S.
References
-
- Yeo et al., Autonomy
- Kirk, Timothy W. “Staying at Home: Risk, Accommodation, and Ethics in Hospice Care.” Journal of Hospice and Palliative Nursing. 16, no. 4 2014: 200-205.
- Yeo et al., Beneficence
- World Health Organization. Constitution of WHO: principles, 2018, http://www.who.int/about/mission/en/. Accessed 30 September, 2018.
H&P From Fall 2018


Reflection
I have mixed feelings about using Blackboard versus CUNY Academic Commons for making my e-Portfolio. I found using the Blackboard platform was difficult in maneuvering around the website. It was difficult to find how to view your page as the author, in comparison with viewing your page as another user. Also, the final view of my page was not as clean as I hoped that it would look. The text that I entered was spilling out of the margins of the page, and there appeared to be no option nor solution to fix this. One pro I found was that entering my post content and uploading the images was straightforward. Another feature I appreciated was the many options available for editing the text.
CUNY Academic Commons’ platform, on the other hand, gave me difficulties with editing my text formats. I had to go through settings to upload a plugin in order to get a feature of being able to change my font type and size. However, if I had to choose between the two platforms, I would choose CUNY Academic Commons. I found it more straightforward to use, as it resembled a lot of how Microsoft Office works. It also makes it easy to go between editing your pages, and viewing how another user would see the page. I also really enjoyed how simple it was to customize the format of my page, and how clean the final product looked. It feels great to be able to add these personal touches.